Kristine Kucera, PA-C, MPAS, DHS
Acne Scarring
Acne is one of the most common inflammatory skin diseases dermatology practitioners encounter. It typically begins at puberty, affecting 95%-100% of adolescent boys and 83%-85% of adolescent girls, and persists into adulthood in approximately 12%-14% of cases. Acne can also emerge, persist, or worsen in adulthood. One of the most distressing and long-term consequences of acne is scarring, affecting up to 95% of patients. For up to 30% of affected individuals, scarring is categorized as severe. These scars are not only aesthetically displeasing but can also result in a significant social and emotional burden. Acne is not just a disease of the face. It is important to ask and examine all areas that may be involved. Truncal acne is a concern not only for active lesions but also because there is a risk for scarring.
The detrimental psychosocial effect of physical acne scarring should be discussed with all patients who are at risk (and their parents). Interventions should be implemented as early as possible to prevent physical scars that may result for inadequately treated acne. If scars are present they are treatment options.
Acne scar development is attributed to an altered wound healing response initiated by cutaneous inflammation—a hallmark of acne. This altered healing response results in an excess of collagen deposition that manifest as hypertrophic scars or–in 80 to 90 percent of cases–decreased collagen deposition that manifest as atrophic acne scars. These atrophic scars can be categorized into three basic types: icepick, rolling, and boxcar, with the icepick type representing 60% to 70% of all acne scars.
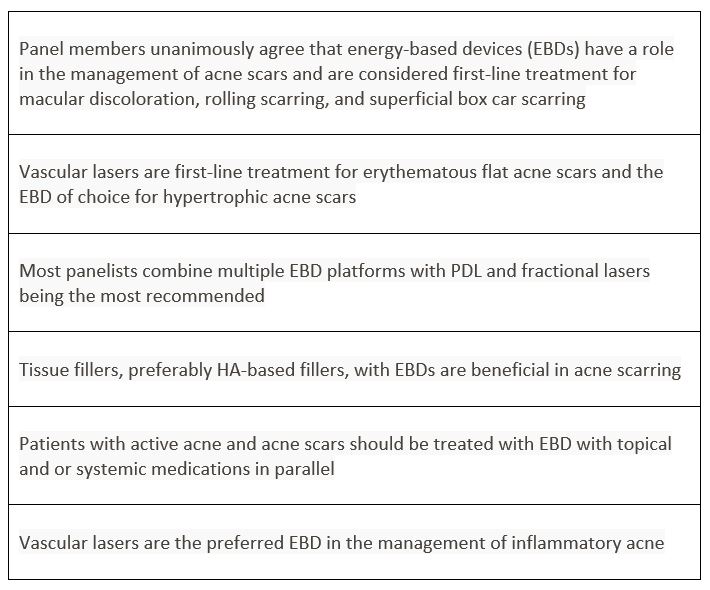
Treatment options for acne scars include surgical (excision, subcision, punch techniques), and nonsurgical approaches (dermabrasion, needling, chemical peels, injectable fillers, energy-based devices). Factors including color, depth, and morphology can affect the treatment choice for each individual scar, and a combined approach may be warranted. Recently for the first time, plastic surgeons and dermatologists from multiple countries collaborated to provide a consensus for treatment using various laser and energy-based devices (EBDs). Published in Lasers in Surgery and Medicine (LSM), the official journal of the American Society for Laser Medicine and Surgery, Inc. (ASLMS), a summary of findings follows as well as a link to the article. Generally, experts agree that various types of EBDs can be first-line treatment for most acne scars and that injectable tissue fillers may play a supportive role in management. The best results may be attained through a combination of modalities to maximize improvement in the skin texture. A common approach is to combine surgical techniques (subcision) and EBD platforms.
SUMMARY OF RECOMMENDATIONS
Kristine Kucera, PA-C, MPAS, DHS, is Assistant Clinical Professor, University of Texas Southwestern, Medical Center PA Program, Dallas, TX. She is a member of the DEF Advisory Council.
References:
International Consensus Recommendations for the treatment of Acne Scars
Energy‐based devices for the treatment of Acne Scars: 2022 International consensus recommendations
(wiley.com)
American Academy of Dermatology
